Slipped Disc /Herniated disc
Introduction to herniated disc
A slip disc, also known as a herniated disc, can cause significant discomfort and disrupt daily activities. Understanding the condition, its causes, symptoms, and treatments can help improve spine health and overall well-being. In this comprehensive guide, we’ll explore the world of slipped discs, discussing everything from causes and diagnosis to herniated disc treatment options.
Understanding Slip Disc
A. Definition and Explanation of Slip Disc
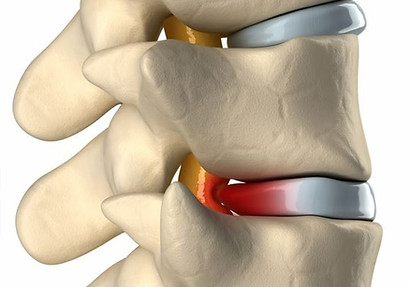
A slip disc, also known as a herniated or bulging disc, occurs when the inner, gel-like nucleus of an intervertebral disc i.e. at the centre pushes through a tear or weak point in the disc’s outer fibrous layer, called the annulus fibrosus. This protrusion can irritate or compress nearby spinal nerves, leading to pain, inflammation, and other symptoms. The term “slip disc” is often used interchangeably with “herniated disc” and “bulging disc,” although these terms may have slightly different meanings depending on the extent of the disc displaced from the center. This condition can occur in any part of the spine, but it is most common in the lower back (lumbar region) and neck (cervical region).
B. Anatomy of the Spine
Vertebrae
The spine, or vertebral column, is composed of a series of individual bones placed one above the other called vertebrae. These bones are categorized mainly into five regions: cervical (neck), thoracic (upper back), lumbar (lower back), sacrum (pelvic), and coccyx (tailbone). In total if you calculate, there are 33 vertebrae, including 7 cervical, 12 thoracic, 5 lumbar, 5 sacral (fused), and 4 coccygeal (fused) vertebrae. Each vertebra has a central hole called the vertebral foramen, through which the spinal cord passes. The vertebrae are connected by facet joints, which allow for movement and flexibility of the spine.
Discs
Intervertebral discs are located between each pair of adjacent vertebrae in the spine. These discs play a crucial role in spinal support, flexibility, and shock absorption. Each disc is composed of two main parts: the nucleus pulposus and the annulus fibrosus. The nucleus pulposus is the soft, gel-like center of the disc, responsible for providing cushioning and shock absorption. The annulus fibrosus is the tough, fibrous outer layer that encases the nucleus and provides structural support to the disc.
In a healthy spine, the intervertebral discs maintain their shape and position, allowing for smooth movement and proper spinal alignment. However, factors such as aging, injury, or lifestyle choices can cause the annulus fibrosus to weaken or tear, leading to a slip disc or herniated disc. This disruption in the disc’s structure can then cause pain and discomfort due to nerve irritation or compression, making it essential to understand and address the factors contributing to slipped discs for optimal spinal health.
III. Causes of Slip Disc
A. Age-related degeneration
As we age, our intervertebral discs undergo natural degenerative processes. Over time, the discs lose hydration, which causes the nucleus pulposus to become less pliable and the annulus fibrosus to weaken. This process, known as disc degeneration, increases the risk of tears and ruptures in the annulus fibrosus, potentially leading to slipped or herniated discs. Slip discs are often caused by age-related degeneration, especially in individuals who are 40 years old or older.
B. Incorrect lifting techniques
Using improper lifting techniques can significantly increase the risk of developing a slipped disc. Bending at the waist or twisting while lifting heavy objects places excessive strain on the spine and the intervertebral discs. To prevent slip discs, it is crucial to adopt safe lifting practices, including bending at the knees, maintaining a straight back, and using the core muscles to provide support while lifting heavy objects. Proper lifting techniques can help prevent injuries to the spine, including slip discs.
C. Traumatic injuries
Accidents and falls can cause traumatic injuries to the spine, resulting in slipped discs. Sudden impacts, such as those sustained in car accidents or sports collisions, can cause the annulus fibrosus to tear or rupture, allowing the nucleus pulposus to protrude. In some cases, these traumatic injuries can cause disc fragments to break off, further exacerbating spinal nerve compression or irritation.
D. Lifestyle factors
Obesity
Carrying extra body weight can impose additional pressure on an individual’s spine and intervertebral discs, potentially raising the chances of experiencing a prolapsed disc. Embracing a wholesome body weight and shedding surplus pounds can aid in lessening the strain on one’s spinal column, consequently diminishing the likelihood of experiencing a herniated disc.
Sedentary lifestyle
Leading a sedentary lifestyle, particularly when it involves long periods of sitting, can contribute to slip disc development. Sitting for extended periods places increased pressure on the intervertebral discs, especially in the lumbar region. Incorporating regular physical activity and movement into your daily routine can help reduce the risk of slipped discs and promote overall spine health.
Smoking
Studies have shown that smoking can have harmful effects on spinal health by reducing the blood flow to intervertebral discs, leading to a lack of crucial nutrients and oxygen. Additionally, the chemicals found in cigarettes can accelerate disc degeneration and weaken the annulus fibrosus, increasing the risk of slipped discs. Quitting smoking can significantly improve overall health and decrease the likelihood of developing spine-related issues.
E. Genetic predisposition
Some individuals may have a genetic predisposition to developing slipped discs. Hereditary elements may contribute to the vulnerability of intervertebral discs to deterioration or damage, influencing their makeup and framework. This can be observed in certain cases. While genetic factors cannot be changed, being aware of this increased risk can help individuals prioritize preventative measures and maintain proper spinal care.
IV. Common Symptoms of Slip Disc
A. Lower back pain
Lower back pain is often the first and most noticeable symptom of a slipped disc. This pain can be sharp, persistent, and may worsen when you move, cough, or sneeze. Many people find that changing positions, applying heat or cold packs, and taking over-the-counter pain relievers can provide temporary relief. It’s essential to listen to your body and avoid activities that cause pain to worsen, as pushing through the pain can exacerbate the issue.
B. Sciatica
Sciatica is a specific type of pain that occurs when a slipped disc compresses or irritates the sciatic nerve, which runs from the lower back down the back of each leg. This can result in a sharp, shooting pain, often described as an electric shock, that travels from the lower back or buttock down the leg, sometimes reaching the foot. Sciatica can be debilitating, making it difficult to walk, sit, or perform daily tasks. Seeking treatment and practicing gentle stretches can help alleviate sciatic pain and prevent long-term complications.
C. Muscle weakness
A prolapsed disc may lead to weakened muscles in the impacted region, hindering the ability to carry out routine tasks like picking up items or ascending stairs. This weakness occurs because the slipped disc disrupts the nerve signals responsible for controlling muscle movement. It’s crucial to address muscle weakness through targeted physical therapy exercises that strengthen the muscles surrounding the spine, as this can help support the affected area and promote recovery.
D. Tingling and numbness
Tingling and numbness are common symptoms of a slipped disc, usually experienced in the area where the spinal nerves are compressed or irritated. These sensations can be unsettling and frustrating, as they can make it difficult to feel or properly use the affected body part. Discussing these symptoms with a healthcare professional can help determine the best course of action to relieve nerve compression and restore sensation.
E. Loss of bladder or bowel function (in extreme situations)
In uncommon and intense cases, a prolapsed disc may result in a condition known as cauda equina syndrome, which arises when nerves at the base of the spinal cord are constricted. This can cause a loss of control over bladder or bowel movements, along with numbness or a tingling sensation in the groin region. This constitutes a medical crisis necessitating prompt intervention and care to avoid lasting nerve harm and impairment. If you encounter these signs, promptly seek medical assistance.
Diagnosing slip disc
In order to diagnose a prolapsed disc, medical practitioners will initially gather a comprehensive medical background and conduct a physical assessment. This may involve particular tests to evaluate muscle strength, reflexes, and neural functioning.
X-rays: to provide additional information about the herniated disc’s location and severity
MRI: for a detailed view of the herniated disc and surrounding tissues
CT scans: to get a clearer picture of the herniated disc’s structure
Electromyography (EMG): to evaluate the degree of nerve damage caused by the herniated disc
VI. Treatment Options for Slip Disc
A. Non-surgical treatments
Pain relief medications
In managing the discomfort associated with a prolapsed disc, utilizing over-the-counter pain alleviating medications like nonsteroidal anti-inflammatory drugs (NSAIDs) can provide short-term respite. Your doctor may also prescribe stronger pain medications or muscle relaxants if necessary. It’s important to use these medications as directed and to communicate with your healthcare provider about their effectiveness in managing your pain.
Physical therapy
Physical therapy plays a vital role in the recovery process for individuals with slipped discs. A physical therapist can design a personalized exercise program to help strengthen the muscles around the spine, improve flexibility, and promote proper posture. These exercises not only alleviate pain but also reduce the risk of future slipped discs. Building a trusting relationship with your physical therapist and committing to your exercise routine can make a significant difference in your recovery journey.
Epidural steroid injections
In some cases, your healthcare provider may recommend epidural steroid injections to reduce inflammation and relieve pain. These injections are administered directly into the affected area of the spine and can provide relief for several weeks or months. Although not a long-term solution, they can offer a much-needed respite from pain, allowing you to engage in physical therapy and other treatments more comfortably.
B. Surgical treatments
Microdiscectomy
If non-surgical treatments fail to provide adequate relief, your healthcare provider may recommend surgery. A microdiscectomy is a minimally invasive surgical procedure that involves removing the portion of the slipped disc causing nerve compression. This procedure has a high success rate and can provide significant relief from pain and other symptoms. Recovery times vary, but most people can return to their daily activities within a few weeks.
Lumbar laminectomy
A lumbar laminectomy, also known as spinal decompression surgery, involves removing a portion of the vertebra called the lamina to create more space for the spinal nerves. This procedure can alleviate pressure on the nerves caused by a slipped disc and may be recommended if more conservative treatments have been unsuccessful.
Artificial disc replacement
In some cases, artificial disc replacement may be an option for those with severely damaged or degenerated discs. This surgery involves replacing the damaged disc with an artificial one, which can restore spinal alignment and alleviate pain. While this procedure is less common than other surgical treatments, it may be considered for specific patients who meet the criteria.
C. Lifestyle modifications
Weight management
Maintaining a healthy body weight can significantly reduce the stress on your spine and lower the risk of slipped discs. Working with a nutritionist or registered dietitian can help you develop a balanced diet plan that promotes weight loss or maintenance while providing essential nutrients for optimal spinal health.
Exercise
Incorporating regular physical activity into your daily routine can help strengthen the muscles that support your spine, improve flexibility, and reduce the risk of slipped discs. Consider low-impact exercises, such as swimming, walking, or yoga, which can be gentle on the spine while still providing numerous health benefits. It’s important to discuss with your medical professional or physiotherapist prior to initiating a new exercise regimen, particularly if you have a past record of prolapsed discs.
Ergonomics
Making adjustments to your work environment and daily activities can help promote proper spinal alignment and reduce the risk of slipped discs. Consider investing in an ergonomic chair, using a standing desk, and taking regular breaks to stretch and move throughout the day. Pay attention to your posture while sitting, standing, and lifting objects, as this can significantly impact your spine’s health.
VII. Prevention Tips for Slip Disc
A. Maintaining a healthy weight
Keeping your weight in check is a simple yet effective way to protect your spine from slipped discs. Excess weight puts additional stress on your spine, which can lead to disc damage over time. By maintaining a well-rounded diet and an active lifestyle, you can foster not only spinal health but also your general well-being. If you’re uncertain about how to begin, seeking advice from a medical expert or nutritionist can guide you towards attaining a healthy weight.
B. Regular exercise
Engaging in regular exercise can work wonders for your spine. By strengthening the muscles that support your spine, you’re better equipped to maintain proper alignment and prevent disc issues. Choose activities you enjoy, such as swimming, walking, or yoga, which are gentle on the spine while still offering numerous health benefits. Keep in mind, it’s always prudent to consult with your medical professional or physiotherapist prior to commencing a new exercise regimen, particularly if you’ve had previous instances of prolapsed discs.
C. Proper lifting techniques
Learning the right way to lift heavy objects can save your spine from unnecessary strain. When lifting, bend at the knees, keep your back straight, and engage your core muscles. This technique helps to distribute the weight evenly, reducing the risk of slipped discs. Moreover, refrain from twisting your body during lifting, as it may exacerbate the damage to your spinal column.
D. Maintaining good posture
Good posture is essential for a healthy spine. Slouching or hunching over can place extra pressure on your intervertebral discs, increasing the likelihood of a slipped disc. Pay attention to your posture while sitting, standing, and even sleeping. You might consider investing in ergonomic furniture or supportive pillows to help maintain proper spinal alignment throughout the day.
E. Taking breaks and stretching during sedentary activities
Sitting for extended periods can take a toll on your spine. It’s crucial to take regular breaks to stand, stretch, and move throughout the day. Set a timer or use an app to remind yourself to get up and move every 30 minutes to an hour. Incorporate simple stretches, such as shoulder rolls, neck tilts, or gentle back twists, to help relieve tension and maintain spinal flexibility.
In conclusion, preventing slipped discs starts with taking care of your spine through healthy habits and lifestyle choices. By maintaining a healthy weight, exercising regularly, practicing proper lifting techniques, focusing on good posture, and taking breaks during sedentary activities, you can significantly reduce your risk of developing slipped discs and promote overall spine health.
